The Concept of the Disease
This is a generic terms for a clinical aggressive tumour of B-cells that does not fall into one the definitive disease categories such as Burkitt Lymphoma or Mediastinal B-cell Lymphoma. This is recognised to be a highly heterogeneous group.
How is it Diagnosed?
Lymph Node or other tissue biopsy
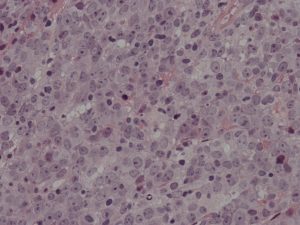
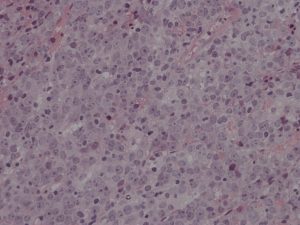
- DLBCL consists of a population of highly proliferative large lymphoid cells which invade and destroy the normal structure of the lymph node or other tissues. About a third of cases present in sites other than a lymph node.
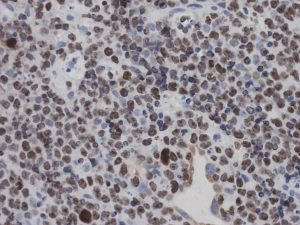
- Almost all cases have an abnormal immunophenotype by flow cytometry and immunocytochemistry.
- Monoclonality is demonstrated by antibody or PCR based techniques.
- Translocations involving MYC, BCL2 and BCL6 are commonly demonstrated using FISH. Abnormalities of a wide range of genes, particularly those involving the NFkB pathway are described.
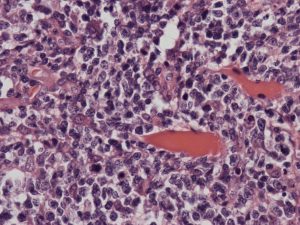
Lymph Node Morphology
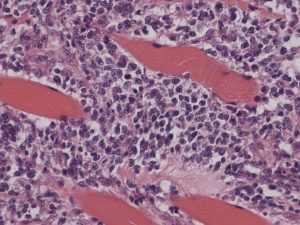
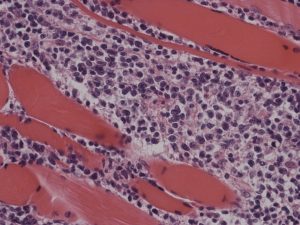
Bone Marrow Trephine Morphology
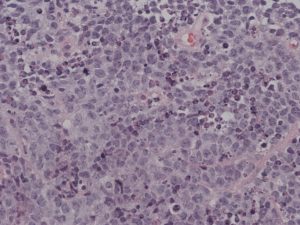
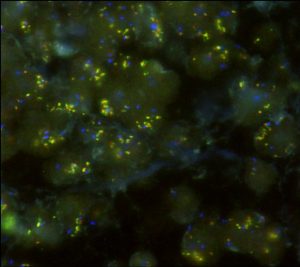
Immunocytochemistry
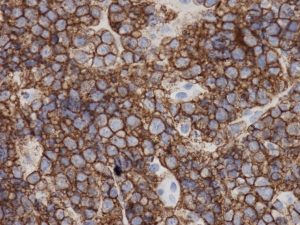
FISH – BCL2 Amplification
What is the Clinical Outcome?
50% of patients treated with R-CHOP chemotherapy are ultimately cured of their disease. However, this masks considerable heterogeneity of outcome.
The International prognostic index (IPI) is the standard method of assessing prognosis at presentation.
| Score | IPI Risk Group |
| 0 – 1 | Low |
| 2 | Low-intermediate |
| 3 | High-intermediate |
| 4 | High |
| Risk Factor | Score +0 | Score +1 |
| Age (years) | ≤60 | >60 |
| Stage (Ann Arbor) | I or II | II or IV |
| Number of extranodal sites | 0 or 1 | >1 |
| Performance Status (ECOG) | 0 or 1 | >1 |
| Serum LDH | Normal | Raised |
Genetic abnormalities such as translocations involving MYC and the sub-classification of the tumour in germinal centre and activated B-cell types using gene expression profiling are also important determinants of outcome.

